Your grandmother lost her sight to glaucoma, and now you wonder if the same fate awaits you. Every time you notice your vision feels a bit off, that worry creeps back in.
Yes, glaucoma can be hereditary, and having a family member with this eye disease significantly increases your risk of developing it too. However, genetics don’t guarantee you’ll get glaucoma — and knowing your family history gives you a powerful advantage for early detection and prevention. The team at Dr. Patricia Fink Optometry helps families understand their glaucoma risk and develop personalized screening plans for eye disease diagnosis and management.
How Family History Affects Your Glaucoma Risk
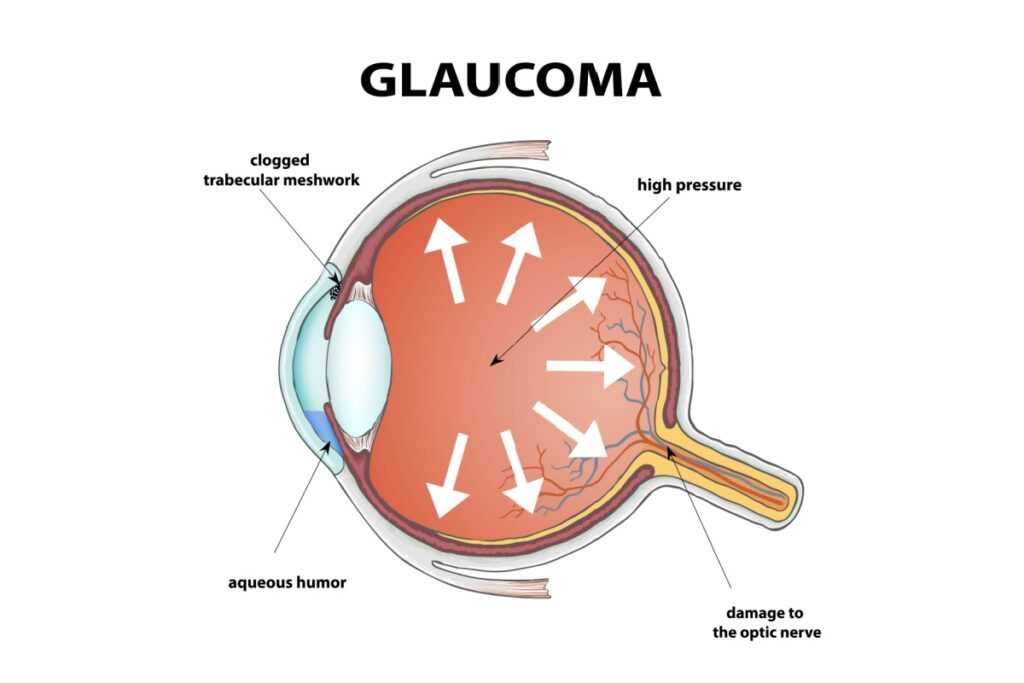
When glaucoma runs in your family, your DNA carries certain genetic variations that make your eyes more vulnerable to this disease. These inherited traits affect how your eye drains fluid and how your optic nerve responds to pressure.
Your relationship to the affected family member matters significantly. Having a sibling with glaucoma carries the highest hereditary risk. Studies show siblings of glaucoma patients face up to nine times the risk of someone with no family history. Parents and grandparents with glaucoma also increase your risk, but to a lesser degree. This difference suggests that epigenetics and shared environmental factors between siblings may play an important role alongside pure genetics.
Age combined with family history creates compounded risk. If you’re over 40 with a family history, your chances of developing glaucoma rise significantly each year.
Types of Glaucoma & Their Genetic Connections
Primary Open-Angle Glaucoma
This most common form shows the strongest hereditary links. Your eye’s drainage system gradually becomes less efficient at removing fluid, leading to increased pressure that damages your optic nerve over time.
Multiple genes contribute to this type, which explains why it often appears in several family members across generations. The disease typically develops slowly and painlessly, making family screening especially important.
Angle-Closure Glaucoma
Your eye’s physical structure — inherited from your parents — determines your risk for this type. People with smaller eyes, thicker lenses, or shallow drainage angles face higher chances of developing angle-closure glaucoma.
This form can develop suddenly and cause severe symptoms like intense eye pain, headaches, and blurred vision. Family members often share similar eye anatomy, putting multiple relatives at risk.
Normal-Tension Glaucoma
Even when your eye pressure stays within normal ranges, genetic factors can make your optic nerve more susceptible to damage. This type often runs in families despite normal pressure readings during routine eye exams.
Your inherited optic nerve structure and blood flow patterns influence whether you develop this form of glaucoma. Regular comprehensive eye exams help catch this type early since pressure alone doesn’t tell the whole story.
Warning Signs You Shouldn’t Ignore
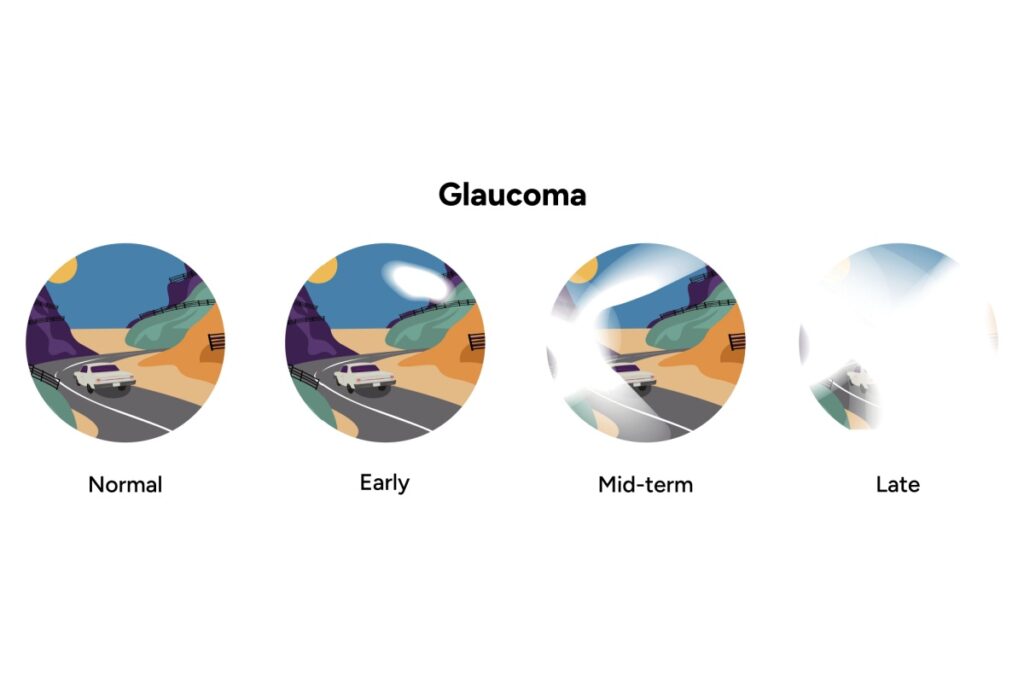
Early detection matters tremendously when you have family risk factors. Most people don’t notice glaucoma symptoms until significant vision loss occurs, making awareness important for your eye health.
- Gradual loss of peripheral vision
- Tunnel vision in advanced stages
- Eye pain or pressure (in some types)
- Halos around lights
- Frequent changes in eyeglass prescriptions
You might not notice these changes happening since they develop slowly. Your brain compensates for vision loss by relying more heavily on your better eye, masking the problem until it becomes severe. If you experience any concerning eye symptoms, seek professional evaluation promptly.
When to Schedule Your Eye Exam in Burlington
Your family history determines how often you need comprehensive eye exams. Starting screenings earlier and more frequently gives you the chance of catching glaucoma before vision loss occurs.
The team at Dr. Patricia Fink Optometry can help you understand your specific risk factors and create a personalized screening schedule based on your family history and other risk factors.
High-Risk Individuals
If you have additional risk factors such as myopia, diabetes, autoimmune disorders, inflammatory conditions, or sleep apnea on top of family history, then annual examinations are strongly recommended regardless of age. A 30-year-old with diabetes and family history needs the same annual screening as someone over 40.
Annual comprehensive eye exams are also essential if you have:
- Multiple family members with glaucoma
- A sibling with glaucoma
- Higher-risk ethnic background (African, Hispanic, or Asian descent)
When multiple risk factors combine, early and consistent monitoring becomes critical. The sooner glaucoma is detected, the better the chance of preventing vision loss over your lifetime.
Moderate Risk Factors
With one family member (parent or grandparent) affected by glaucoma and no other risk factors, glaucoma screening can be done every two years after age 40, then annually after 60. However, your overall eye health needs may require more frequent comprehensive exams. Your eye doctor will recommend an exam schedule that addresses all your vision and health needs, not just glaucoma risk.
What Happens During Glaucoma Screening
A comprehensive glaucoma screening involves several specialized tests that work together to give us a complete picture of your eye health. Understanding what to expect can help you feel more comfortable during your appointment and appreciate the thoroughness of the evaluation.
Eye Pressure Measurement (Tonometry)
We measure the pressure inside your eye using specialized equipment. While elevated pressure is a major risk factor for glaucoma, it’s not the only indicator. Some people develop glaucoma with normal pressure (normal-tension glaucoma), while others have elevated pressure without developing the disease. That’s why we never rely on pressure alone.
Optic Nerve Examination
Using OCT (optical coherence tomography) scanning and retinal photography, we carefully assess your optic nerve for signs of damage. These imaging technologies allow us to compare your results over time, detecting subtle changes that indicate glaucoma progression.
OCT scans are particularly valuable because they can detect nerve fiber layer loss years before it shows up on visual field testing. Since a person needs to lose 30% of their nerve fiber layer before it becomes visible as a visual field defect, OCT gives us a critical window for early intervention. If damage is occurring, OCT can detect changes within 6 months, allowing us to adjust treatment before permanent vision loss occurs.
This is why we keep your retinal images on file from childhood onward. When you have a family history of glaucoma, establishing baseline images early and tracking any changes throughout your life gives us the best chance of catching the disease at its earliest stages. Those childhood images become an invaluable reference point for comparison decades later.
Visual Field Testing (Perimetry)
This test maps your complete field of vision to detect any blind spots or areas of vision loss. You’ll focus on a central point while indicating when you see lights appear in your peripheral vision. The results create a detailed map showing exactly where vision loss has occurred, often revealing damage before you notice it yourself.
Angle Examination (Gonioscopy)
We examine the drainage angle where fluid exits your eye. This assessment helps determine your risk for angle-closure glaucoma and guides treatment decisions. The test involves placing a special contact lens on your eye to view the internal structures that control fluid drainage.
These tests work together to detect glaucoma early and monitor its progression over time. Regular testing allows us to compare results year after year, catching subtle changes that indicate the disease is developing.
Steps You Can Take Beyond Genetics
While you can’t change your genetic makeup, you can influence other factors that affect glaucoma development. These lifestyle choices work alongside regular eye exams to protect your vision.
Manage Blood Pressure and Perfusion
Both high and low blood pressure can increase glaucoma risk, but for different reasons. What matters most is perfusion pressure – the blood flow reaching your optic nerve.
People with low blood pressure (hypotension) face particular risk for normal tension glaucoma. If you tend to feel dizzy or faint when standing too quickly (often called POTS), you’re at higher risk. The biggest concern is during sleep, when blood pressure naturally drops even further, reducing perfusion to the optic nerve and causing nerve fiber layer loss overnight. This is why some people with high blood pressure who take medications at night and lie down to sleep can paradoxically develop the same perfusion problems as the hypotension group – their blood pressure drops too low.
Sleep apnea compounds this issue by disrupting oxygen delivery during those critical nighttime hours. Inflammatory conditions like diabetes and autoimmune disorders also affect blood vessel health and perfusion.
Regular cardiovascular exercise improves overall blood flow and eye health. However, if you have blood pressure concerns in either direction, work with your doctor to optimize your levels and protect optic nerve perfusion.
Protect Your Eyes from UV Damage
Wear quality sunglasses that block 100% of UVA and UVB rays. While the direct link between UV exposure and glaucoma isn’t conclusively established, there are some suggestions that oxidative stress from excessive UV light may increase the inflammatory response around the optic nerve head.
Another possibility is that UV exposure accelerates cataract formation, which thickens the lens and pushes it forward, narrowing the drainage angle and increasing eye pressure. Regardless of the mechanism, UV protection remains an important part of overall eye health.
Manage Other Health Conditions
Keep diabetes, sleep apnea, high blood pressure, and other systemic conditions well-controlled. These conditions affect blood flow to your optic nerve and can compound your genetic glaucoma risk. High blood pressure is particularly concerning if you take medications at bedtime, as nighttime blood pressure dips can reduce optic nerve perfusion.
Myopia is another important risk factor. This is why children with family history should have regular imaging starting early – as myopia increases, so does glaucoma risk. Tracking both conditions over time gives us the clearest picture of your child’s long-term eye health needs.
These proactive measures work alongside your screening schedule to give you the best chance of preserving your vision.
The Role of Stress and Overall Wellness
Clinical observations over decades suggest that chronic stress and tension may play a role in glaucoma development. Many glaucoma patients tend to be meticulous, detail-oriented individuals who carry tension throughout their body. Managing stress through relaxation techniques, regular exercise, and mindfulness may help support your overall eye health, particularly if you have other risk factors.
Your eye health reflects your overall health. Studies have even shown changes in foot pressure and gait patterns before glaucoma diagnosis occurs, reinforcing the interconnected nature of body systems. Taking care of your mental, emotional, and physical health supports your vision in ways that extend beyond traditional risk factors.
Follow Treatment Consistently
If diagnosed with glaucoma, use prescribed eye drops exactly as directed. Missing doses allows pressure to rise and damage to progress. Consistent treatment is crucial for preventing vision loss.
Modern Treatment Options for Glaucoma
Glaucoma treatment has advanced significantly in recent years. Eye drops have traditionally been used to lower eye pressure and preserve the optic nerve, but they don’t address the underlying drainage problem.
First-line treatment is now often SLT (Selective Laser Trabeculoplasty) or ALT (Argon Laser Trabeculoplasty), which have proven more effective at improving drainage. Pressure-lowering eye drops are now mainly used as adjunct treatment. Great advances have also been made with MIGS (Microinvasive Glaucoma Surgery) for more advanced cases.
Your optometrist plays an important role in co-managing your glaucoma care. While laser treatments and surgical procedures are performed by ophthalmologists, your optometrist can prescribe and adjust glaucoma medications, monitor your condition between specialist visits, and ensure continuity of care. This collaborative approach means you have consistent access to the care and medication management you need.
The key is early detection – the earlier glaucoma is caught, the more treatment options are available and the better the outcomes.
Protect Your Vision with Proactive Care
Your family history doesn’t have to determine your future. While you can’t change your genetics, early detection and consistent monitoring give you the best chance of preserving your vision for life.
At Dr. Patricia Fink Optometry in Burlington, we provide comprehensive glaucoma screening and ongoing monitoring for families with hereditary risk. Our thorough approach combines advanced diagnostic technology with careful tracking over time to catch changes before they affect your daily life.
Don’t wait for symptoms to appear – by then, permanent damage may have already occurred. Book your comprehensive eye exam at Dr. Patricia Fink Optometry in Burlington to establish your baseline and create a personalized screening plan that protects your vision for years to come.